There is growing evidence that the Brazilian butt lift (BBL) is the cosmetic surgery procedure with the highest incidence of death. This has set off alarm bells among board certified Plastic Surgeons. These deaths are primarily occurring due to Pulmonary Fat Embolisms (PFE). I have been performing this procedure safely for 15 years and the new data emerging about the increased mortality rates is disturbing.
I have been studying the issue closely and will do my best to explain what I see happening, and also discuss ways to increase patient safety. I believe the recent mortalities with this procedure can be dramatically reduced to have no greater risk than any other cosmetic surgery procedures. However, this not only involves standardization of some surgical techniques, but also requires patients to rigorously vet the credentials of both the surgeon and the surgical facility.
Recent statistics and reported deaths
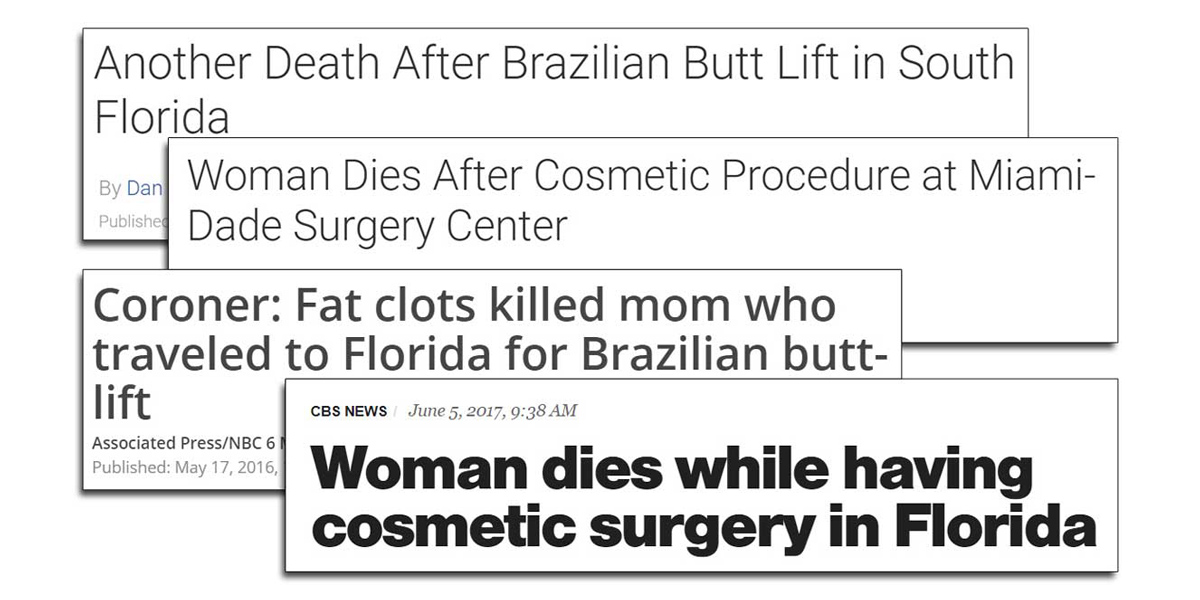
Media reports over the past couple of years detail many BBL tragedies to include those described here, here, and here. The most recently reported tragedy was just last week. A significant number of these recent deaths have taken place in Florida.
Equally troubling is the fact that most of the recently reported deaths in Florida were surgeries performed by non Plastic Surgeons. These doctors advertise themselves as ‘Cosmetic Surgeons,’ but they did not complete a residency in plastic surgery. The medical specialty which teaches principles of both liposuction and fat grafting during the residency program is ‘plastic surgery’.
In addition, in some of these publicly reported cases, the surgical facility was not accredited.
Pulmonary fat embolism, PFE
Reviewing the recent media coverage about BBL mortalities, as well as available published literature, the majority of deaths occurred from a condition called Pulmonary fat embolism, or PFE.
PFE is a mechanical blockage of the pulmonary veins by fat particles.
Previously, PFE’s were predominantly characterized as a rare complication of orthopedic surgery, but they can also occur with a direct injection of adipose tissue, as is the case with BBL. Pulmonary fat embolism is not to be confused with Fat embolism syndrome. The syndrome disease is a systemic inflammatory response that can often be managed successfully.
The pulmonary fat embolism (PFE) is a mechanical blockage of the pulmonary veins by fat particles. It occurs when an injection cannula injures a vein, allowing injected adipose fat to enter the vein and block it. The fat particles can also travel through the pulmonary veins to the heart. While not all PFE’s are fatal, many do result in death within the first 24 hours following surgery.
Publications & task force teams

The plastic surgery community was first alerted to the risk of pulmonary fat embolism in a paper published in the Plastic and reconstructive journal in 2015 by Dr. Lazaro Cardenas-camarera, et al.
The 2015 Cardenas-camera et al publication
“Deaths caused by gluteal lipoinjection: What are we doing wrong?” discussed a series of deaths that had occurred over the past 15 years in Mexico and Columbia. The conclusion of this paper was that intramuscular gluteal lipoinjection is associated with mortality caused by gluteal blood vessel damage during fat injection:
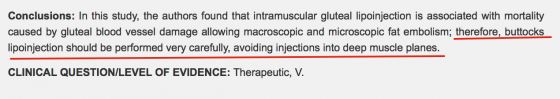
In other words, the paper concluded that injecting fat into the gluteal muscles increased the risk of pulmonary fat embolism.
The ASERF paper and task force
Then, in 2016, a Task Force was created by the Aesthetic Surgery Education and Research Foundation (ASERF), to study these PFE complications. An anonymous survey was sent to 4,853 Plastic Surgeons around the world and the data was analyzed. The results of the survey were published in early 2017 by M. Mark Mofid, MD et al. in the Aesthetic surgery journal.
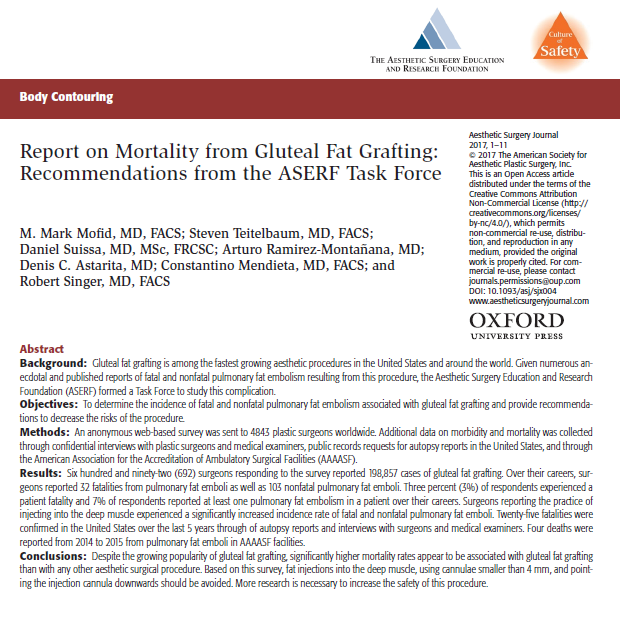
The data determined that the probability of having either a fatal or non fatal pulmonary fat embolism was 1:1473 (one in 1,473). Furthermore, the risk of death was estimated to be 1:3448 (one in 3,448).
To put this in perspective, the risk of death from any cosmetic surgery procedure in an accredited AAAASF facility is 1:55000 (one in 55,000). Prior to this paper, the highest known mortality rate associated with an aesthetic procedure was abdominoplasty, with a mortality rate of 1:13147 (one in 13,147).
In summary, the risk of mortality with a Brazilian Butt Lift was estimated to be 3 times higher than any other cosmetic surgery procedure and 16 times higher on average than any type of procedure performed in an accredited surgery center. These results were shocking.
2017, a Multi-society gluteal fat grafting task force
After the Mofid paper was published, another task force team was established to study the issue further. This new task force team invited 19 plastic surgeons from ASPS, ISPRES, ISAPS, and ASAPS, and IFATS.
The multi-society task force team of surgeons studying gluteal fat grafting is a combination of plastic surgeons who have been performing the BBL for many years, as well as academic leaders in the field of Plastic Surgery. I was honored to be selected as a member of this task force.
In the Spring of 2017, we began meeting to evaluate the ASERF report findings as well as study the autopsy reports of patients who have died due to Pulmonary Fat Embolism. Our discussions are ongoing and I am not at liberty to share details, but I do want to put my thoughts forward in hopes of educating patients further and helping to avert any harm possible.
So, please note, my comments are not a statement of the task force, but are rather my own opinion based on years of experience, review of the retrospective publications, and examination of autopsy reports.
Reducing the risk of PFE during BBL procedures – my own thoughts
I believe there are a number of contributing factors leading to PFE, and that board certified plastic surgeons can reduce risk factors and make the procedure less risky for their patients. Having performed well over 200 Brazilian butt lifts with not a single patient requiring overnight hospitalization, I feel confident that these measures dramatically reduce risk.
Patients contemplating a Brazilian butt lift procedure should be aware of the risks, specifically the risk of PFE, and should consider the following to minimize the risk involved. As a BBL patient, you should be sure to:
- Choose a board certified plastic surgeon
(American Board of Plastic Surgery) - Have your surgery performed in an accredited surgery center
(AAAASF, JCAHO) - Ask your surgeon about injection technique details
- Are the injections performed in the subcutaneous or intramuscular plane?
- How many cc’s are injected in each pass?
- How long will the lipoinjection take?
- Has he/she read the ASERF report and recent publications about mortality in BBL?!
- Use IV sedation with tumescent solution instead of general anesthesia
Choose a board certified plastic surgeon
Let’s start with the obvious. Do not pick your surgeon solely based on his/her SnapChat and Instagram videos!!
Do not pick your surgeon based on Instagram and SnapChat videos!
Likewise, it’s not all about patient reviews, as these can be gamed and paid for. While those may factor into your final decision, the most important criteria is the proper training of your plastic surgeon. The goal is safety above everything.
Over the past 15 years, I have observed a steady increase in other Medical Specialties advertising Brazilian butt lift procedures. This includes not only OB/GYN, but also non-surgical medical specialties like family medicine. Recently publicized deaths have indeed included doctors from these medical specialties. Some of these doctors are board certified, but they are not board certified in plastic surgery which means they are performing the procedure without proper training because there is a high demand and patients are willing to pay for the service.
The only ABMS approved residency training program that teaches Liposuction and Fat transfer is ‘Plastic Surgery.’
The Brazilian butt lift procedure involves both:
- Liposuction
- Fat transfer/Fat injections
The only ABMS (American Board of Medical Specialties) approved residency training program that teaches Liposuction and Fat transfer is ‘plastic surgery.’ The board certification is from the American Board of Plastic Surgery. This is very different from the ‘American Board of Cosmetic Surgery.’ There is no ABMS Residency in ‘cosmetic surgery.’ It is NOT the same.
Furthermore, attention should also be given to the credentials of your anesthesiologist. He or she should be board certified by the ‘American Board of Anesthesiology.’
Why choose a surgeon board certified in plastic surgery?
First, plastic surgery residents are introduced to the vast libraries of medical publications on various plastic surgery procedures, and they discuss these publications routinely. These publications include details of complications and risks. Their professors have authored many of these publications during their academic tenure.
An autologous fat transfer is a completely different ball game than injecting Restylane or Juvederm.
Residents assist in performing procedures under full supervision of attending surgeons for many years. In addition there is much time spent on studying and analyzing how to avoid and manage complications!
Finally, during their senior year, many surgical residents in plastic surgery training programs have the ability to travel and visit other experienced plastic surgeons to learn particular procedures. For example, in my practice here in Baltimore, the Johns Hopkins Plastic Surgery residents have been rotating through my surgery center to watch and learn the Brazilian butt lift procedure for years!
An autologous fat transfer is a completely different ball game than injecting Restylane or Juvederm. Taking a one week course on Liposuction and simply visiting a ‘famous’ doctor who performs the procedure, does not cut it for performing a Brazilian butt lift.
The plastic surgery residency program is a 6 year training process. A plastic surgery resident gets to experience the entire breadth of plastic surgery procedures and learns about related complications and how to avoid them – all while under the supervision of an experienced board certified plastic surgeon. This process takes years of hard work and study. It is not a weekend course.
Finally, surgeons who are board certified by the American Board of Plastic Surgery are eligible to become a member of the ASPS.

Annual ASPS conferences have presentations on BBL complications and techniques and discuss ways to improve the procedure. Publications and abstracts are presented on complications, and surgeons openly discuss ways to improve surgical results and safety. Doctors from other medical specialities do not have access to this ASPS dialogue!
Check here to find out if your plastic surgeon is board certified by the American Board of Plastic Surgery.
Have Your BBL performed in an accredited surgery center
Before you blindly trust that your surgeon will be using an accredited surgery center… ask! Accreditation means that the facility has strict protocols and credentialing requirements in place for the surgeon, OR staff, and the anesthesia provider. Written protocols are in place for licensing, malpractice insurance, instrument sterilization, equipment maintenance, back up generators, life safety protocol, emergency protocols, infection control, and a whole host of other vitally important topics. Accreditation also means that the facility is inspected by the agency on a regular interval.
In the USA, the surgery center should be accredited by either the AAAASF, JCAHO, or Medicare. You should see a current certificate of accreditation on the wall. If not, you should consider that a red flag.
In addition, do not be afraid to ask if both your surgeon AND the surgical facility carry malpractice insurance. If you have your procedure in Florida, you will find out that this is (shockingly) not mandatory.
Ask your plastic surgeon about the injection process
The most consistent finding about risk of increased mortality from both task force teams and the 2015 Cardenas-Camarera, et al publication was that injecting in the deep muscles of the gluteal area increases risk of injury to the vessels. The recommendation is to inject into the subcutaneous space, which is the area above the muscles, and avoid injecting deep into the muscle.
Where does your surgeon inject? Has he heard of the ASERF report?
Likewise, do not be afraid to ask your plastic surgeon about how he performs the fat injection process. Ask if injections will be made into the deep muscles or the subcutaneous planes. All of the evidence so far suggests that there is a greater risk of vein injury when injections are performed into the deep muscles below the subcutaneous region. Injections should be performed in the subcutaneous region, which is the area closest to the skin.
If your surgeon gets vague or cagey with these questions, this is a red flag. Read further to understand why.
Gluteal vasculature anatomy
The gluteal region is a very vascular structure. Vascularity means that there are a lot of blood vessels and arteries below the surface in the buttocks area.
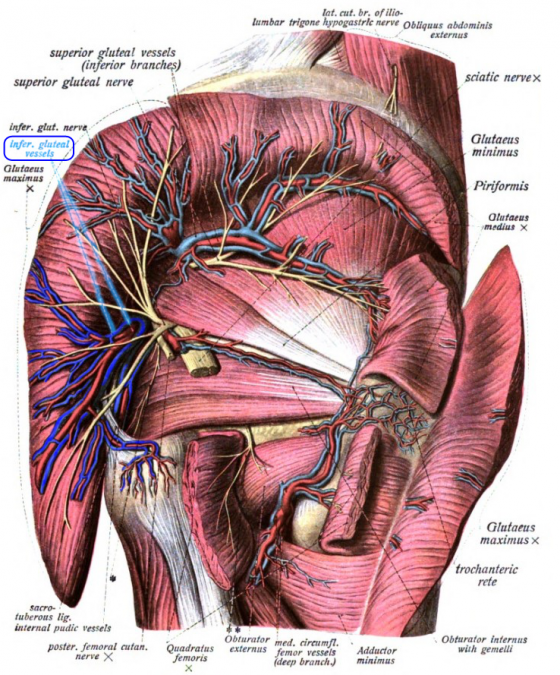
Look at the diagram of the gluteal vasculature shown here. The veins are shown in blue and the arteries are shown in red in the buttock.
Unless your plastic surgeon is using an ultrasound probe while he injects, he can NOT see these veins while he is injecting. He must know where the arteries are and where the danger areas are.
Pulmonary fat embolism (PFE) occurs when a vein wall is injured during the injection process thus allowing fat to enter the vessel. The most dangerous area is where the inferior and superior gluteal veins emerge from the pelvis to the gluteal muscles. This area must be avoided.
How much fat is injected in each injection pass?
Reliable and safe fat grafting has been around for several decades, and was pioneered by Dr. Sydney Coleman. His technique is considered the gold standard of fat grafting across the field of plastic surgery. Its hallmarks are: a) Centrifugation of fat to remove impurities, 2) Use of thin, blunt tip injection cannulas 3) Low injection pressure, and 4) Injecting small deposits of fat at each pass of the injection cannula. Plastic surgery residents learn these standardized methods during their Residency.
For many years, fat transfers were limited to small volumes and were primarily focused on face and breast shape defects. Only in the recent decade have patients requested very large volumes of fat injected into each buttock cheek with the Brazilian butt lift. These high volumes are a new development in fat graft practice. Historically, average fat volumes for BBL procedures have been approximately 400cc in each buttock cheek, as summarized in a retrospective meta analysis paper by Dr. Alexandre Conde Green published in 2016.
I do not think the total volume of fat injected necessarily creates increased risk of PFE. However, I do think that injecting a large volume of fat all at once (in the same injection pass) creates large clumps of fat that can then get into a vein and create a blockage. I believe that injecting small volumes of fat (1-3 cc) at many different injection locations largely eliminates the risk of large chunks of fat blocking a vein.
Many surgeons, looking for a competitive edge in pricing and shorter operating times, have abandoned the safe and reliable Coleman technique in favor of speedy injection techniques.
Nowadays, total injection amounts are commonly approaching 800-1000cc per cheek. If a plastic surgeon uses conventional fat grafting techniques standardized by Dr. Sydney Coleman, these large volumes increase the length of surgery to somewhere between 5-7 hours. That also increases the cost of surgery. Many surgeons, looking for a competitive edge in pricing and shorter operating times, have abandoned the safe and reliable Coleman technique in favor of speedy injection techniques.
With power injection methods, instead of injecting 1-3 cc’s per pass, surgeons are now injecting 60cc’s to hundreds of cc’s per pass. In my opinion, this can NOT be good. This is like slamming as much fat into the buttock as quickly as possible. There is no way to know exactly where the major veins are beneath the surface, and there is no way to know exactly where your cannula is under the skin. It stands to reason that dumping a lot of fat at one time into an unknown space is a recipe for disaster.
Injecting into the subcutaneous space

The best way for a surgeon to minimize any possible damage to the gluteal veins is to place the cannula so that the they know exactly where the tip of the cannula is. The way I do this is by pushing the cannula tip right up to the skin so that I can see the cannula tip tenting the skin, and I can feel the tip directly under the skin. I know where my cannula tip is at all times. Look at the image above to see the cannula tip near the surface. This is the only way to be sure that the cannula tip is in the subcutaneous space right under the skin and away from the danger area of the gluteal veins.
Since the fat comes out at the cannula tip, this ensures the fat is deposited in the superficial subcutaneous space in your buttock. Any other method can only really guess where the cannula tip is. Even injecting in a plane parallel to the table can result in injury to the vein and depositing fat in the intramuscular plane. If you are injecting a lot, or injecting very quickly with a power injection tool, there is no time to pull out or even ‘feel’ what you are doing. If you hit a vein, it’s too late. It is really important to note that in the most recent cases of PFE, the surgeons thought they were injecting in a superficial subcutaneous space.
Use IV sedation anesthesia instead of general anesthesia
In April 2016, a publication from Alexandra Conde-Green in Plastic and reconstructive journal concluded, among other things, that most Brazilian butt lifts are performed under general anesthesia. Her analysis included 4,105 BBL patients from 17 publications.
While it is widely known that General Anesthesia carries a much higher incidence of pulmonary embolism (PE) compared to IV sedation, I believe that general anesthesia also increases the risk of pulmonary fat embolism (PFE). Let me explain why . . .
General anesthesia causes vasodilation. Vasodilation basically means that the veins enlarge. In addition, the machine that breathes for you during general anesthesia uses positive pressure ventilation (PPV) to push air into your lungs. This pushes the blood inside the chest out into the peripheral veins, which also dilates the peripheral veins.
I do not think Brazilian butt lifts should be performed under general anesthesia.
– Dr. Rodriguez
The problem is that when performing a BBL under general anesthesia, the veins get bigger, therefore presenting a larger target for injury and an easier pathway for fat to flow into! This is a recipe for pulmonary fat embolism.
With IV sedation (TIVA) plus the use of tumescent solution, the opposite happens. The veins actually get smaller. With this type of anesthesia, it is harder to injure the veins and harder for fat particles to enter the smaller diameter pathways!
For these reasons, I do not think this procedure should be performed under general anesthesia. I have been using IV sedation for BBL’s for many, many years. In fact, here I am at our 2017 national meeting in Orlando speaking on the ASPS BBL safety panel. There are 5 other plastic surgeons on this panel including Drs. Conde-Green and Dr. Coleman.
This short clip captures the moment when I was speaking about how IV Sedation should be used instead of general anesthesia. I know that you will be hearing more about this in the future!
The safest way to perform the Brazilian butt lift is using the gold standard in fat grafting techniques and IV sedation combined with tumescent analgesia.
– Dr. Rodriguez
In summary, the safest way to perform the Brazilian butt lift is using the gold standard in fat grafting techniques (small cannulas, small fat deposits, low pressure injection) and IV sedation (TIVA) combined with tumescent analgesia. If you are considering BBL surgery, please be aware of the risks and choose your surgeon with great care. Make sure he is Board Certified by the American Board of Plastic Surgery. Ask questions. Where does he inject? Has he read the ASERF report? If you get a blank stare it is not a good sign. Asking all of the right questions will help ensure you’re choosing the right surgeon to trust your life with.
When performed with correct techniques by well-credentialed surgeons, I continue to believe that the Brazilian butt lift procedure is safe and that patients can achieve beautiful results with the procedure. If you have any questions about your surgeon’s credentials, please be sure to ask them here.